Mastering the Art of Fusion - Independent Summaries of Success
- Paradigm Biodevices Inc.
- Our Blog
- Hits: 6852
BY MATTHEW O'NEILL
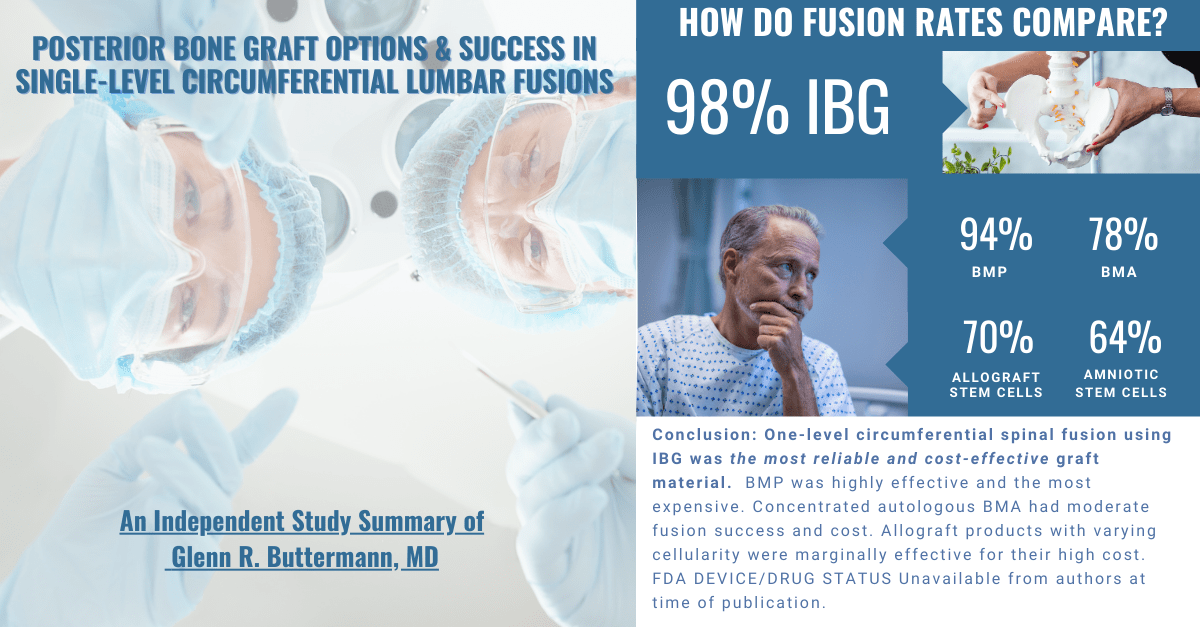
Since the 1990s, the orthobiologics marketplace has morphed into a 5 billion dollar1 insatiable beast, devouring precious health care resources while producing mediocre fusion results at gargantuan expense. An abundance of recent independent clinical data has shown that not one bone graft alternative has surpassed autogenous iliac crest graft in either fusion rate success or safety and efficacy. It is hard to rationalize how some may opt for bone graft alternatives contributing to a higher non-union rate at great expense. If these products contribute to sub-optimal results, is there a better solution? It is widely accepted, and clinically-proven, that autograft is the indisputable “gold standard.” ICBG is the master of osteogenesis that delivers the best results and is the benchmark for all others.
Donor site morbidity and complications have been prevalently reported in historic clinical data, which is often 30 to 40 years old. One example is that of Younger & Chapman, et al, published in 1989. 2 This data reports findings collected from 1982 to 1985 which has been cited thousands of times in current scholarly articles and numerous marketing sources. This outdated data is used to stoke fear of autografting and promote the use of alternative bone graft substitutes . Pain and morbidity described in these old studies center around bone grafting techniques involving the removal of large cortico-cancellous wedges and large structural bone grafts that require massive gluteal stripping and blunt trauma to the iliac crest. These methods have since been replaced with advances in spine surgical techniques which have come a long way since the 1980s, as have MIS iliac crest bone grafting techniques.
Multiple recent independent peer reviewed studies confirm that MIS ICBG techniques are safe, reliable, and cost effective for surgeons seeking to maximize fusion success, reduce expense, and garner meaningful reimbursement. These studies demonstrate the success of modern MIS ICBG techniques. These include:
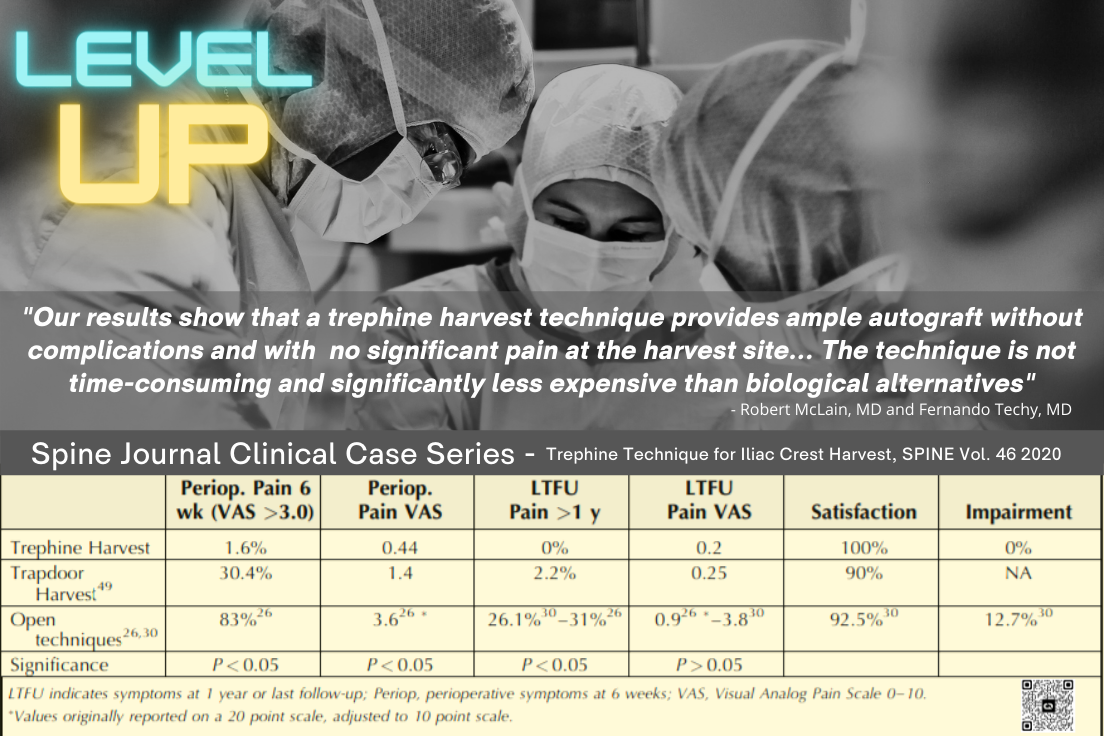
Trephine Technique for Iliac Crest Bone Graft Harvest (R. McLain, SPINE 2020 ) found that less invasive techniques have been shown to reduce perioperative complications and pain, but contemporary orthopedic literature still advocates a traditional open harvest for anterior crest harvest.”3 MIS trephine techniques that utilize a gluteal sparing stab incision have made autograft attainable without the previously described drawbacks. McLain et al. reviewed 68 consecutive patients, and reported "...there were no graft site infections, hematomas, wound dehiscence recorded in any patient… No patient reported either moderate or severe graft site pain at any time … All patients expressed (100%) satisfaction with the graft harvest aspect of their surgery.”4
Another independent study, Does Iliac Crest Bone Graft Harvest Really Cause Significant Pain (A. Pearson, Spine Journal 2019) found “Concern about iliac crest bone graft harvest site morbidity has helped create a massive bone graft substitute industry and prompted many spine surgeons to use local bone graft and bone graft substitutes instead of ICBG, despite ICBG resulting in better fusion rates."5 The study reported that only “24% of patients consistently and correctly identified the ICBG site over the first year following surgery. There were no significant differences in median iliac crest pain scores between the harvested and intact iliac crests at any follow-up point, and iliac crest pain scores correlated with midline low back pain scores.”6
Of equal importance, Postoperative Pain Following Posterior Iliac Crest Bone Graft Harvesting in Spine Surgery: A Prospective Randomized Trial, (E. Sheha, Spine Journal 2017) discovered that “many postoperative spine patients may have pain in the vicinity of the posterior iliac crest that may not in fact be caused by bone graft harvesting.”7 The randomized investigation showed “while pain on the surgical side was slightly higher, it was neither clinically nor statistically different from the non-surgical side.”8 The study noted “current literature does not adequately ililluminate the incidence of post-operative back pain at the site of harvest and the relative magnitude of this pain in comparison to the patients' residual low back pain…Our conclusion supports surgeons’ use of autologous bone graft, which offers cost-effective, efficacious spinal fusion supplement.”9
Similar findings were prevalent in another independent study, A retrospective study of iliac crest bone grafting techniques with allograft reconstruction: do patients even know which iliac crest was harvested? (S. Pirris, Journal of Neurosurgery 2014) which reviewed 25 patients who underwent iliac crest autografting with allograft reconstruction. They found that 64% of patients could not identify which side had been harvested post operatively. The investigators noted that “Autograft site pain has led many companies to develop an abundance of bone graft extenders, which have limited proof of efficacy.”10
In conclusion, fusion patients should be given the best possible opportunity for a good outcome including a bone graft that can deliver the highest fusion rate with minimal potential for complication. A suboptimal bone graft can negate any advantages obtained with a technologically advanced spinal implant technique. Progress in MIS autografting techniques is delivering relevant results for surgeons and patients as is witnessed in the above clinical studies. A closer examination of this data demonstrates that successful fusion rates and limited probability of pain is reliably attainable. ICBG remains the gold standard and is a safe and potent option for physicians and patients.
1Bruder, Scott. “True Progress in Orthobiologics Requires That We ... - Azisks.” True Progress in Orthobiologics Requires That We Police Ourselves and Each Other, 2020. https://www.azisks.com/wp-content/uploads/2020/09/AAOS-NOW-BIOLOGICS-3.pdf.
2Younger, Edward & Chapman, Michael “Morbidity at Bone Graft Donor Sites.” Journal of Orthopaedic Trauma. U.S. National Library of Medicine, 1989. https://pubmed.ncbi.nlm.nih.gov/2809818/.
3McLain, Robert. “Trephine Technique for Iliac Crest Bone Graft Harvest...: Spine.” LWW, 2020. https://journals.lww.com/spinejournal/Abstract/2021/01010/Trephine_Technique_for_Iliac_Crest_Bone_Graft.12.aspx.
4Ibid.
5Pierson, Adam. “Does Iliac Crest Bone Graft Harvest Really Cause Significant Pain? : Spine.” LWW, 2019. https://journals.lww.com/spinejournal/blog/spineblog/pages/post.aspx?PostID=583.
6Ibid.
7Sheha, Evan. “Postoperative Pain Following Posterior Iliac Crest Bone Graft Harvesting in Spine Surgery: a Prospective, Randomized Trial.” The Spine Journal, 2017. https://www.thespinejournalonline.com/article/S1529-9430(17)31062-8/fulltext.
8Ibid.
9Ibid.
10Pirris, Stephen. “A Retrospective Study of Iliac Crest Bone Grafting Techniques with Allograft Reconstruction: Do Patients Even Know Which Iliac Crest Was Harvested? Clinical Article.” Journal of neurosurgery. Spine. U.S. National Library of Medicine, 2014. https://pubmed.ncbi.nlm.nih.gov/25014500/.